Key Points
Despite the mandating of shelter-in-place rules as of 07 January 2021, the Center for Disease Control’s (CDC) Ensemble Forecast indicates 405K–438K deaths in the U.S. alone related to COVID-19 by the end of January 2021.
Sponsored by the U.S. Government’s Operation Warp Speed (OWS), to date the bio-pharma companies have done an outstanding job of developing and now producing a vaccine for COVID-19. However, due to the lack of understanding and application of fundamental and simple Operations Science, State and Local Governments are struggling to deploy the vaccines.
Using a rate of ~1 vaccine per min, with ten administers working in 50 locations per state, the US should be able to deploy tens of millions of vaccines a month, and in a few months, achieve herd immunity.
The healthcare sector’s reliance on scheduling (i.e., using appointments) rather than a robust flow-based production system is causing a delay in efficient vaccine deployment, thus leading to unnecessary deaths as well as wrecking parts of the economy. In other words, vaccines are piling up while customers and in this case, all of us as the patients, suffer. Meanwhile, the economy continues to be damaged, and State and Local Government officials remain confused.
The key to eradicating the virus now rests with understanding and applying fundamental, but simple, Operations Science, to effectively and rapidly deploy the vaccines to all in our society. In other words, the State and Local Government officials who constantly explain that they are applying “data and science” to solve this problem, will, along with their constituents, benefit from the use of real science – Operations Science. Doing so will solve the problem, save millions of lives and bring us back to “a normal state.”
Background
The idea of “flattening the curve” is predicated based on the strategy that measures are put in place (lockdowns, wearing of PPE, social distancing, etc.) to buy time until a vaccine can be researched, developed, tested, approved, distributed and administrated. Early on, the majority of populations were diligent in following Federal, State and Local Government guidelines related to flattening of the curve, while the U.S. Government launched Operation Warp Speed.
To date, U.S. bio-pharma companies (as well as several others non-US based companies) have successfully developed and produced vaccines for COVID-19. However, State and Local Governments are currently struggling to effectively deploy the vaccines.
Discussion
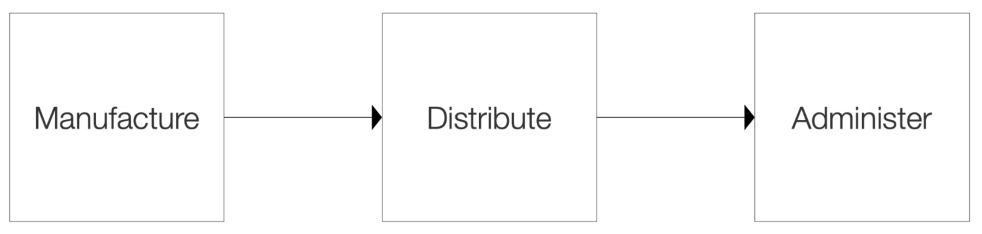
At the most basic level, the deployment of a vaccine requires three primary operations: 1) manufacture the vaccine, 2) distribute the vaccine and 3) administer the vaccine. With the manufacture and distribution of the vaccine being executed by global leaders in the fields of pharmaceutical manufacturing, transportation and logistics as well as pharmaceutical distribution, it appears sufficient throughput of vaccines is moving through the process. However, the last operation in the process, known as ‘the last mile’ in the world of supply chain management, is struggling to achieve the necessary throughput.
Based on the approach being used by State and Local Governments, this struggle should not come as a surprise. Sadly, the implications are unacceptable including unnecessary destruction of the economy, and more importantly, illness and death (from not only contracting COVID-19, but also from the psychological implications of others dying, businesses being shuttered, etc.).
But further analysis indicates that there are many reasons as to why Administer is the bottleneck in the process. This includes the fact that some States didn’t believe a vaccine could be produced by end of 2020, while some States made it a political issue claiming they would protect their citizens by establishing a panel of experts to validate the efficacy and safety of the vaccines. But perhaps, the most impactful of all is the lack of understanding and application of fundamental and simple Operations Science principles to understand how the production process and its operations for deployment of a vaccine behave.
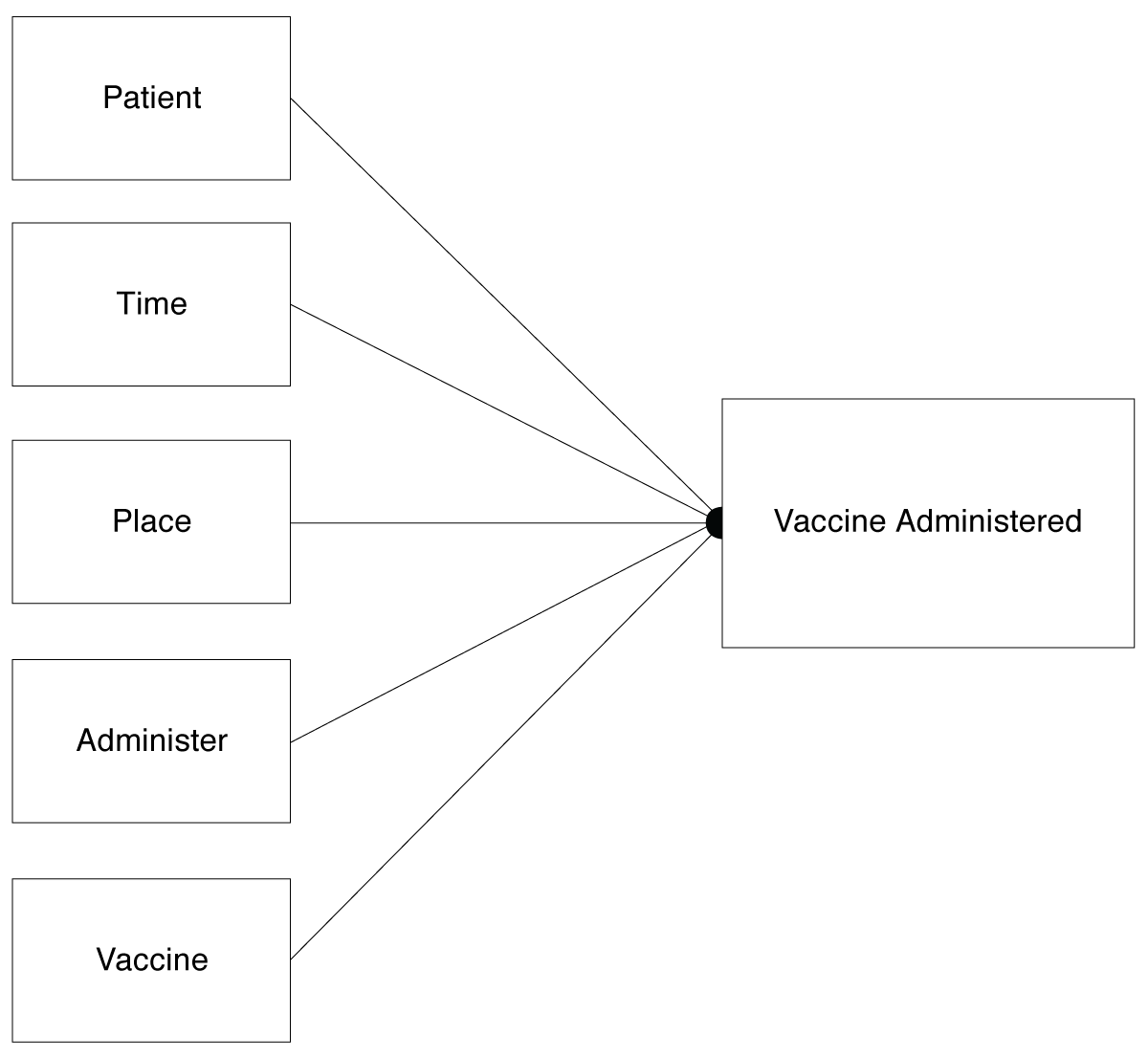
When scheduling is used as the means to manage a production system, including the deployment of a vaccine, those doing it need to address a self-imposed “matching” problem. In the case of COVID-19 vaccines, the match is between five different elements: 1) having a patient available to receive the vaccine, 2) a scheduled time to administer the vaccine, 3) a place to administer the vaccine, 4) a person to administer the vaccine and 5) having the vaccine itself along with the associated equipment needed to administer it. If any one of these don’t go per the schedule, other elements are forced to adjust which creates additional changes and results in an unstable system. If each of these requirements are available 90% of the time, the likelihood of all five being available is reduced to less than 60%.
A more effective means of doing this is to start by understanding that the goal is to achieve “herd immunity” through vaccinating as many people as possible in the least amount of time. From an Operations Science perspective, the key measurement is Throughput or TH – the total amount of work accomplished for a given period of time. Achievement of the maximum throughput requires that process be efficient (meaning no unnecessary steps), inventory and capacity are effectively controlled and variability effectively managed.
The desire to use scheduling coupled with the need for matching as outlined above, increases variability in the overall vaccine deployment process. Any increase in variability results in less throughput for the same available resources. The unintended consequence is the discard of vaccines due to shelf life and, more importantly, unnecessary loss of life.
Therefore, eliminating the time element of the match, while dedicating places and people to administer the vaccines, will dramatically increase the throughput or total number of people being vaccinated. While there will always be a need for the patient, the vaccine and the administrator to be in the same place at the same time, there is no need to try to specify those times and places beforehand. Given live information about current queues, patients will go where they believe they can be served the most quickly. Thus, self-selection, and not scheduling, will remove this bottleneck and contribute to increase throughput to achieve “herd immunity”.
The important decision then becomes how much vaccine to have at each administration point. Again, this should not be scheduled, but should be in response to current demand. In other words, there should be a given amount of vaccine either on hand or in transit that is required to meet current demand. Operations Science provides the mechanics for understanding how much inventory is needed in a way that meets demand without having so much that vaccine is kept past its shelf life. In Operations Science, this is called a flow production system where eliminating the scheduling of appointments coupled with dedicated capacity (people and place) and dynamic inventory control reduces variability and allows for buffering of variability when it does occur.
What to Go Do Now
Our leaders and their scientific experts have informed us over and over that the most important goal is to achieve herd immunity, and the means for doing so is to rapidly create, make and administer a vaccine. If this is truly the case, then in reality not much data is needed, other than that related to efficacy and safety of the vaccines as well as data related to deployment of the vaccine. All other data is of limited use. Based on this, there are five specific strategies that can be made operational:
Reconsider the appropriateness and effectiveness of the tiered approach and focus on the goal of achieving herd immunity through maximum throughput of people vaccinated, while continuing to use other strategies such as continued shelter in place to protect high-risk people.
Forego the desire to schedule / use appointments and instead use dedicated resources (administers and places) to administer the vaccine. Do not use hospitals and other healthcare facilities to administer vaccines. If distribution logistics can accommodate, do not use “super centers” to administer vaccines – use small and more geographically disperse centers.
Use retinal scanning or other standard off-the-shelf biometric data capture systems to monitor who has and has not been vaccinated.
Synchronize vaccine deployment with vaccine manufacture and distribution as the means to avoid the unnecessary creation of inventories that may affect the shelf life of the vaccines.
Identify and manage the bottleneck. Based on the handling and storage requirements, manufacturing should be the designated bottleneck (not distribution and administer). In other words, have extra capacity at the distribution and administer points. This would mean that there would be times when these resources would be idle for lack of patients and this would be deliberate. But that is better than having people turned away for a lack of vaccine or having vaccine thrown away due to its expired shelf life.
